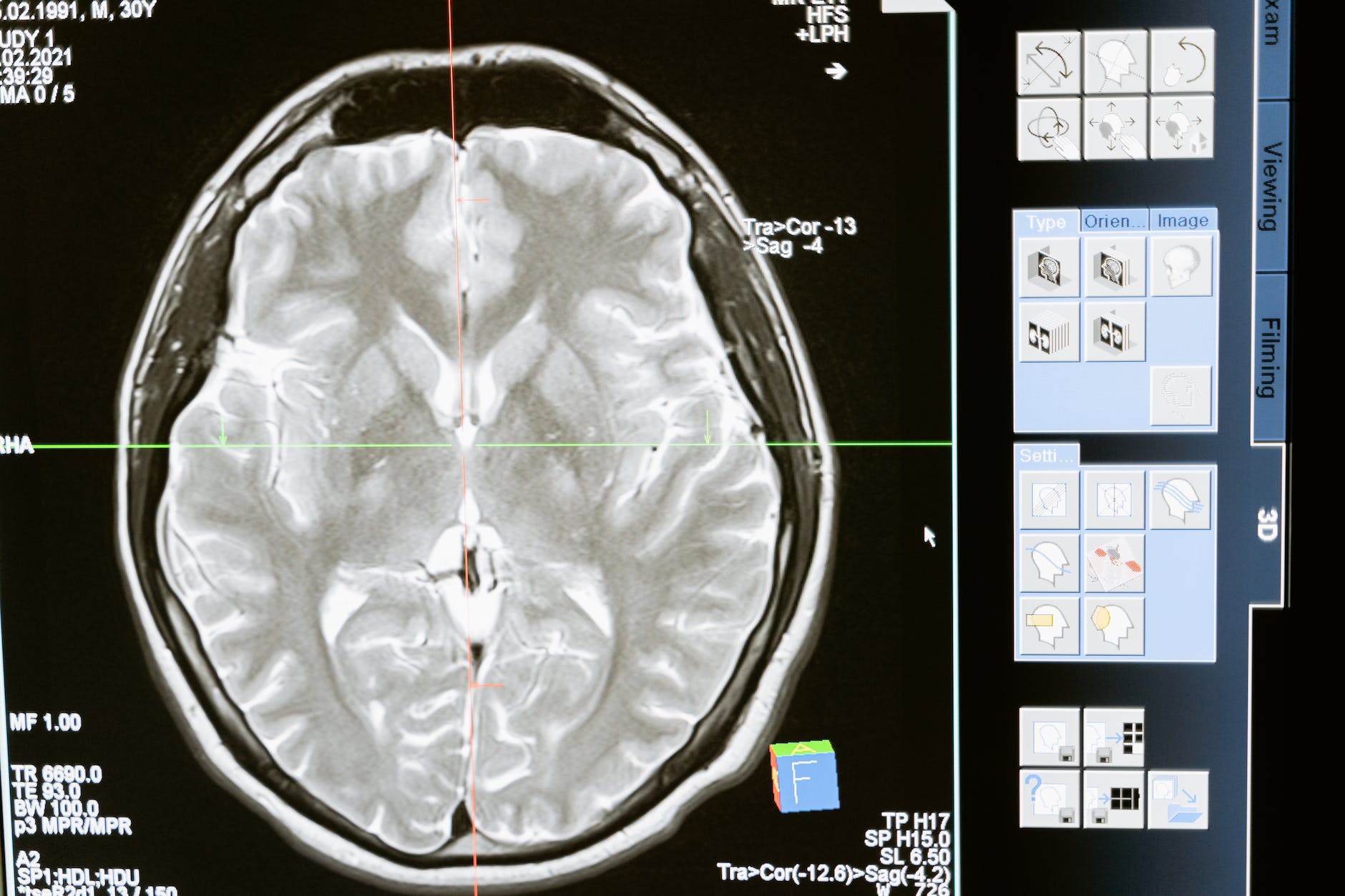
Brain
Navigating the journey of brain tumor treatment can often feel like a labyrinth. It’s a path laden with medical terminology, challenging decisions, and emotional upheaval. Yet, amidst these complexities, a beacon of hope emerges in the form of integrative care. By weaving traditional medical treatments with complementary therapies, this approach creates a tapestry of care addressing the whole person: body, mind, and spirit.
This article highlights how integrative approaches can enhance brain tumor treatment, fostering a holistic care experience.
The Power of Integrative Medicine
Integrative medicine is a rapidly expanding field that marries conventional medical treatments with complementary therapies. This approach is about treating the whole person, not just the disease. It’s a philosophy particularly beneficial for brain tumor patients, who often grapple with various physical and emotional challenges.
Focusing on the patient can help address these challenges in a comprehensive manner, enhancing the overall quality of care and potentially improving outcomes. It’s a powerful approach that recognizes the interconnectedness of all aspects of health and the importance of addressing all these aspects in a coordinated way.
The Neurosurgeon’s Role in Brain Tumor Treatment
The neurosurgeon plays a pivotal role at the heart of brain tumor treatment. Embarking on the intricate terrain of the brain, these medical experts perform surgeries with the potential to profoundly influence a patient’s prognosis. Yet, they don’t work in isolation. They’re part of a broader ensemble that includes oncologists, radiologists, and an increasing number of practitioners specializing in complementary therapies. This growing emphasis on a multi-disciplinary approach is reflective of a larger trend in the medical world.
Adoption and Global Prevalence of Integrative Medicine
Integrative medicine’s adoption is on the rise globally, with medical institutions increasingly recognizing its holistic value. In the U.S., leading institutions like the Mayo Clinic and the Cleveland Clinic have established integrative medicine centers. Similarly, complementary therapies have been integrated into healthcare systems in Europe and Asia for decades. The World Health Organization also acknowledges the value of such practices. (Source: MedNEXT J Med Health Sci, 2021) However, adoption rates vary by region due to cultural beliefs, regulatory environments, and professional availability.
The global prevalence of integrative medicine is driven by patient demand for personalized treatments, growing evidence supporting complementary therapies, and the recognition of health’s multi-dimensional nature.
Complementary Therapies: More Than Just a Band-Aid
Complementary therapies aren’t intended to replace traditional treatments. Instead, they’re designed to work in conjunction with them, helping manage symptoms, reduce side effects, and improve overall well-being. These therapies can include practices like acupuncture, which can help manage pain and nausea; massage therapy, which can alleviate stress and promote relaxation; and mindfulness meditation, helping patients cope with anxiety and depression.
Integrating these therapies into the treatment plan can offer patients additional tools to navigate their journey with brain tumors. It’s about providing a more comprehensive approach to care, recognizing the value of both conventional and complementary therapies.
The Mind-Body Connection
In health and healing, the profound connection between the mind and body is crucial. Techniques like mindfulness meditation, yoga, and biofeedback can help patients manage stress, reduce anxiety, and improve their quality of life during treatment. Mindfulness meditation, for instance, can help patients stay present and focused, reducing feelings of fear and uncertainty. Yoga can improve physical strength and flexibility while promoting relaxation and stress relief. Biofeedback can help patients gain control over bodily processes that are usually involuntary, such as heart rate, helping them manage symptoms and improve their overall well-being. Recognizing and leveraging the mind-body connection can offer a more comprehensive and effective approach to care.
Nutrition: Fuel for The Fight
Good nutrition is essential during brain tumor treatment. It can help patients maintain their strength, cope with side effects, and support their immune system. A registered dietitian can provide personalized advice, assisting patients to make dietary choices that support their overall health and well-being. This can include advice on maintaining a balanced diet, managing dietary side effects of treatment, and using nutritional supplements safely and effectively.
Focusing on nutrition can ensure they’re giving their bodies the fuel they need to fight the disease and recover from treatment. It’s a crucial aspect of integrative care that recognizes the important role of diet in health and healing.
The Role of Exercise
Exercise can be a powerful tool for brain tumor patients. It can help manage fatigue, improve mood, and enhance physical function. Of course, talking to your healthcare team before starting any new exercise regimen is essential. But with proper guidance, patients can incorporate physical activity into their routine safely and beneficially. This can include activities like walking, stretching, or strength training. Regular exercise can also help patients manage stress and improve their overall quality of life, making it an important component of integrative care. It’s about recognizing the value of physical activity in health and healing and helping patients incorporate it into their lives.
The Importance of Emotional Support
Dealing with a brain tumor can be emotionally challenging. Support groups, counseling, and psychotherapy can provide a safe space for patients to express their feelings, cope with fear and anxiety, and connect with others who are going through similar experiences. These resources can provide emotional support and practical advice, helping patients navigate the emotional aspects of their journey. Healthcare providers can ensure that patients aren’t only surviving but also thriving. It’s about recognizing the vital role of emotional health in overall well-being and providing the support and resources patients need to navigate this challenging journey.
Education and Training in Integrative Medicine
The instruction of healthcare professionals in integrative medicine is a key element of this comprehensive approach. Research in the journal ‘Evidence-Based Complementary and Alternative Medicine’ indicates that as medical students progress in their studies, they’re more likely to view their education in complementary and alternative medicine (CAM) as sufficient. This implies that as students delve deeper into their studies, their comprehension and exposure to integrative approaches grow.
However, the research also underscored that the quality of education related to CAM varies greatly. Some students expressed that their CAM-related education was biased, either favoring or opposing CAM. It was of relatively lower quality than the rest of their medical education. This highlights the necessity for a consistent and more informed strategy for teaching future doctors about integrative medicine.
Personal Use of Complementary and Alternative Medicine
Interestingly, the research disclosed many medical students reported personal experiences with CAM. Almost half of the respondents had used CAM for self-treatment, and 38% had received treatment from a CAM provider. The most frequently used CAM therapies included massage, deep breathing exercises, prayer for health reasons, yoga, meditation, diet-based therapies, herbal medicine, progressive relaxation, aromatherapy, and non-vitamin, non-mineral, natural products.
This personal application of CAM among medical students could shape their attitudes towards integrative medicine, potentially making them more receptive to suggesting such approaches to their future patients.
The Future of Integrative Care In Medical Education
Looking ahead, the prospects for integrative care within medical education are bright. Research indicates that while medical students seem open to the foundational principles of CAM, they might view CAM therapies as lacking a solid evidence base. This underscores the necessity for further investigation, especially studies that probe into CAM therapies’ mechanisms, safety, and cost-effectiveness. Furthermore, the research highlights the importance of a more thorough and uniform approach to teaching CAM to medical students.
As medical curricula have been updated to reflect the dynamic nature of medicine and incorporate new disciplines, it’s crucial for medical educators to acknowledge the significance of training future physicians in healthcare practices that extend beyond traditional medicine.
Integrative Medicine in Pain Management and Quality of Life Improvement
Integrative medicine plays a significant role in managing pain, particularly in patients dealing with chronic conditions such as brain tumors. Combining conventional medical treatments with complementary therapies provides a more comprehensive approach to pain management. This approach aims to alleviate physical discomfort and improve patients’ overall quality of life.
For instance, a joint guideline published by the ‘Society for Integrative Oncology and the American Society of Clinical Oncology’ provides evidence-based recommendations on integrative medicine for cancer pain management1. The guideline recognizes the potential of integrative medicine to resonate with diverse cancer populations and fill existing gaps in pain management.
Evidence-Based Complementary Treatments
With the growing demand for holistic therapies, the emphasis on scientifically validated complementary treatments becomes paramount. The National Center for Complementary and Alternative Medicine (NCCAM) categorizes complementary and alternative medicine (CAM) into five main groups: comprehensive medical systems, mind-body wellness, biologically based, manipulative and body-focused therapies, and energy fields.
However, not all therapies under these categories have definitive proof of their efficacy and safety. Therefore, relying on those with substantial evidence supporting their use is essential. This ensures that patients receive treatments that aren’t only holistic but scientifically validated.
Models of Integrative Medicine
Two dominant models of integrative medicine exist. The Supplementary Model selectively combines complementary therapies with conventional treatments. In contrast, the Collaborative Model incorporates only well-researched complementary treatments into standard care.
These models offer different levels of autonomy, control, and responsibility among the participating health professionals. Despite their differences, both models focus on the patient and provide a holistic approach to care.
A well-designed model of integrative medicine that combines every possible means and every available treatment, including all necessary safety checks, can be particularly effective in achieving the goal of any medical system. This goal is the comprehensive treatment of the disease and its side effects across all aspects of the patient’s life.
Conclusion
Navigating brain tumor treatment can indeed be a daunting task. However, the emergence of integrative approaches to care offers a more holistic pathway to recovery. Combining traditional medical treatments with complementary therapies can aim to treat the whole person’s body, mind, and spirit. As research continues and medical education evolves, we expect to see even more innovative and effective integrative treatments emerge, providing patients with a more comprehensive and holistic care experience.






